Beneficiaries
We should all be tested for HIV regularly.
Luckily, getting an HIV test in South Africa is easy, whether you’re on a medical scheme or not.
If you get a result that shows you’re HIV positive, call AfA straight away on 0860 100 646.
Our staff are trained to help you with what comes next, and you can rest assured that help is 100% confidential.
What to expect from AfA once you’re registered on the programme
Once you’ve been diagnosed:
- Make an appointment with your doctor.
- With your doctor’s assistance, complete and submit an AfA registration form. Download the form here.
- AfA will process your registration and contact you once it’s finalised.
- Once you’re registered, we’ll walk you through managing your condition:
-
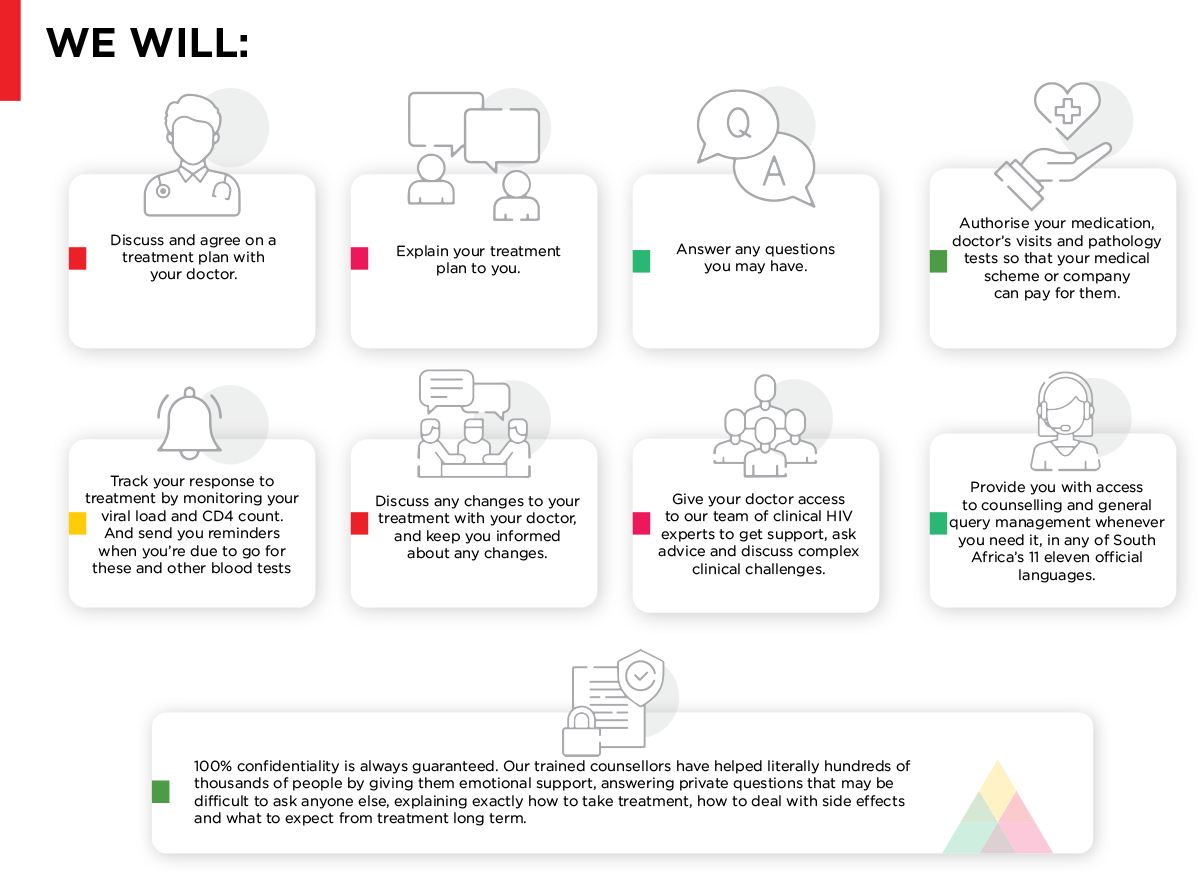
- We will discuss and agree on a treatment plan with your doctor.
- We will explain your treatment plan to you.
- We will answer any questions you may have.
- We will authorise your medication, doctor’s visits and pathology tests so that your medical scheme or company can pay for them.
- We will monitor your viral load and CD4 count to track your response to treatment. And we’ll send you reminders when you’re due to go for these and other blood tests.
- If your treatment needs to be adjusted, we will discuss this with your doctor, and keep you informed about any changes.
- We give your doctor access to our team of clinical HIV experts to get support, ask advice and discuss complex clinical challenges.
- We provide you with access to counselling and general query management whenever you need it, in any of South Africa’s 11 eleven official languages. 100% confidentiality is always guaranteed. Our trained counsellors:
-
-
- provide emotional support;
- answer personal questions that may be difficult to ask anyone else; and
- explain exactly how to take treatment, how to deal with side effects and what to expect from treatment long term.
-
REGISTRATION
Registering on the AfA programme is easy:
- Make an appointment with your doctor.
- Your doctor will examine you and help you complete the form.
- Fax your completed form to AfA on our toll-free number:
0800 600 773 or send an email to afa@afadm.co.za. - AfA will process your registration and contact you once it’s finalised.
REGISTRATION FORMS
- AfA registration form: Registration form for HIV+ patients requiring ART.
- AfA PEP registration form: Registration form for post-exposure prophylaxis.
- AfA PrEP registration form: Registration form for HIV- patients requiring PrEP
- Patient consent form for telephonic/internet registration: Consent form for patients enrolled telephonically, or via direct online processing.
LIVING WITH HIV
Stigma around HIV can lead to discrimination, fear and denial. Fortunately, South Africa has been at the forefront of tackling HIV stigma for many years. Policies have been implemented in the workplace nationally to protect the rights of those living with HIV.
All South Africans have access to preventative methods, diagnosis through testing, care and treatment thereby making the right to accessible healthcare a priority. Government, business and communities have become good at having conversations about HIV and providing support to those who need it.
But how can you remove the fear and stigma out of an HIV diagnosis for yourself? We tend to stigmatise those things that we don’t fully understand.
AfA is here to help you demystify HIV and unpack some of the things that may cause you to be fearful.
FREQUENTLY ASKED HIV QUESTIONS
I’ve just been diagnosed with HIV.
I feel overwhelmed and confused about what’s involved in managing my condition.
We understand – AfA is here to help you every step of the way.
Once you’ve been diagnosed:
- Make an appointment with your doctor.
- Together, fill out, sign and submit an AfA registration form. You or your doctor can download the form here.
- AfA will process your registration, and we’ll contact you as soon as it’s finalised.
- Once you’re registered, we’ll walk you through every step of managing your condition.
I’ve heard about antiretroviral treatment – is it effective?
The short answer is, yes! That’s because your viral load can change ...
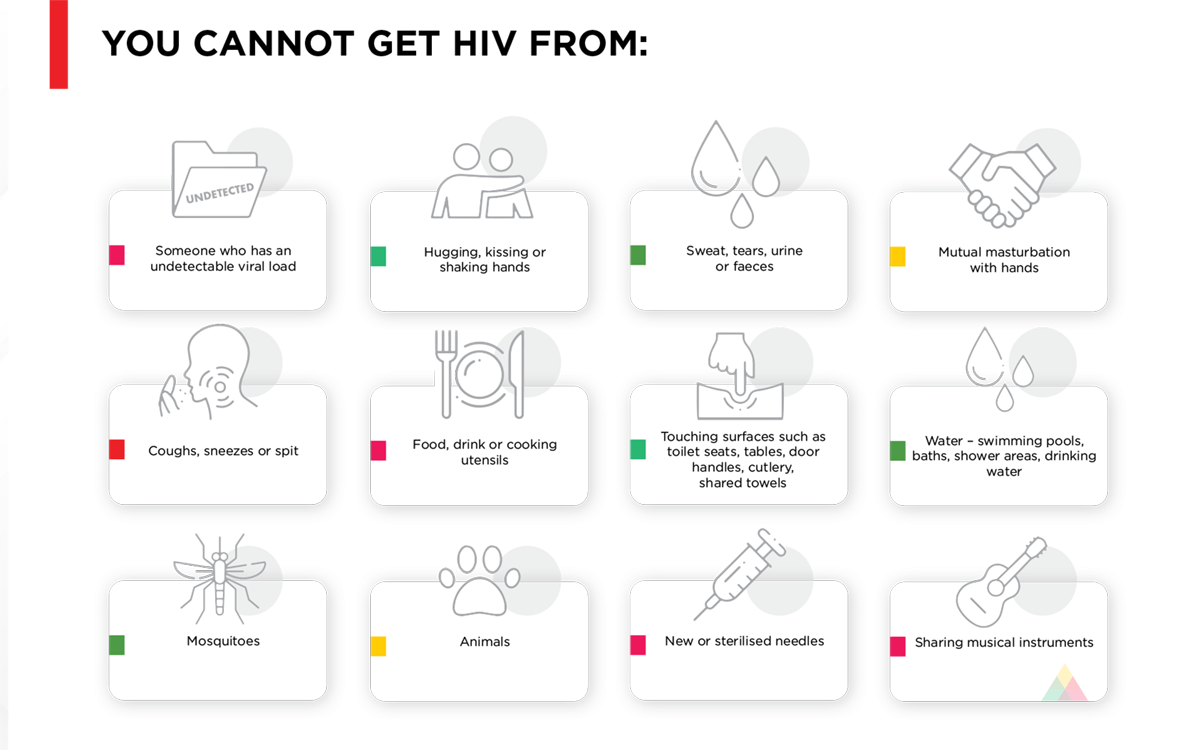
In fact, antiretrovirals can lower viral load in your blood to the point that it’s undetectable. When that happens, not only can you live a healthy, productive life but you won’t be able to transmit the virus to another person.
If you test regularly for HIV, start taking antiretroviral treatment as soon as you’re diagnosed and stick to your prescribed treatment regimen, the antiretrovirals will lower the ‘load’ of virus in your blood.
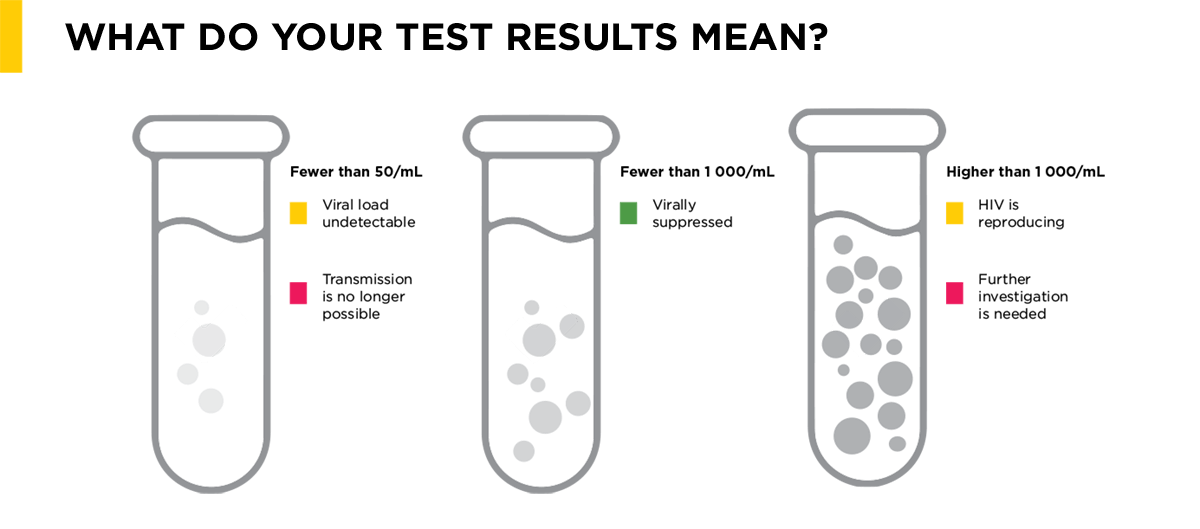
Some numbers you need to know when it comes to monitoring your viral load and the effectiveness of your antiretrovirals:
• Once your viral load result is lower than 1 000/mL, you are virally suppressed.
• Once your viral load result is lower than 50/mL, your viral load is undetectable, meaning that you cannot pass the virus on to another person.
It’s important to remember that your viral load will only reduce and stay reduced if you take your medicine exactly as prescribed. So is antiretroviral treatment effective? Absolutely!
Undetectable = Untransmissable
If someone living with HIV is managing their condition well under the guidance of a doctor and the ‘load’ of the virus in the blood (viral load) has been suppressed through antiretroviral treatment to the point of being undetectable (this can only be confirmed by your doctor after a blood test), they will no longer be able to pass the virus onto another person. It is still always important to practice safe sex by using condoms however as a suppressed viral load will not protect you against other sexually transmitted diseases.
What about relationships and sex after an HIV diagnosis?
Finding out that you’re HIV positive can trigger a range of emotions and thoughts about what your life will look like going forward. It’s quite normal to feel overwhelmed. One thing that most people worry about is relationships. You may think you can never have a relationship again or that sex will never be an option for you. None of these things is true – people living with HIV fall in love, have sex, find fulfilling relationships, marry and have children – all without passing on HIV.
Some people self-stigmatise after getting an HIV diagnosis. This is when people living with HIV start to have thoughts and beliefs that they are infectious, not desirable and not worthy of experiencing pleasure and intimacy. Remember that whatever you are feeling is part of the process of adjusting to your diagnosis. The shock experienced after your diagnosis is temporary and your response to living with HIV will change as you learn how best to manage it. AfA’s counsellors are available to you when you feel you need support in processing negative feelings. They have years of experience and knowledge that can really help you to deal with both emotional and practical aspects of receiving an HIV diagnosis and the impact that has on your relationships.
Here are a few practical things for you to consider:
- Deciding when and how to tell a partner can be difficult. Remember that it’s your choice how much you tell them and when. But it’s also your responsibility to have the discussion before you engage in sexual activity together.
- Always use a condom when you have sex. When used properly, condoms are still the easiest, most effective way of protecting against HIV and other sexually transmitted diseases.
- Make sure you understand about the impact of having an undetectable viral load and discuss this with your partner.
- Read about PrEP and discuss the potential benefits with your partner. PrEP is for people who are HIV negative and can protect them against HIV infection.
- Don’t forget about contraception. Condoms protect against HIV and STI infection but also unwanted pregnancies. Discuss additional contraception methods with your partner and a healthcare professional. It’s important to tell your healthcare professional if you’re taking HIV treatment and contraceptive drugs together as some antiretrovirals interact with other drugs and can make them less effective.
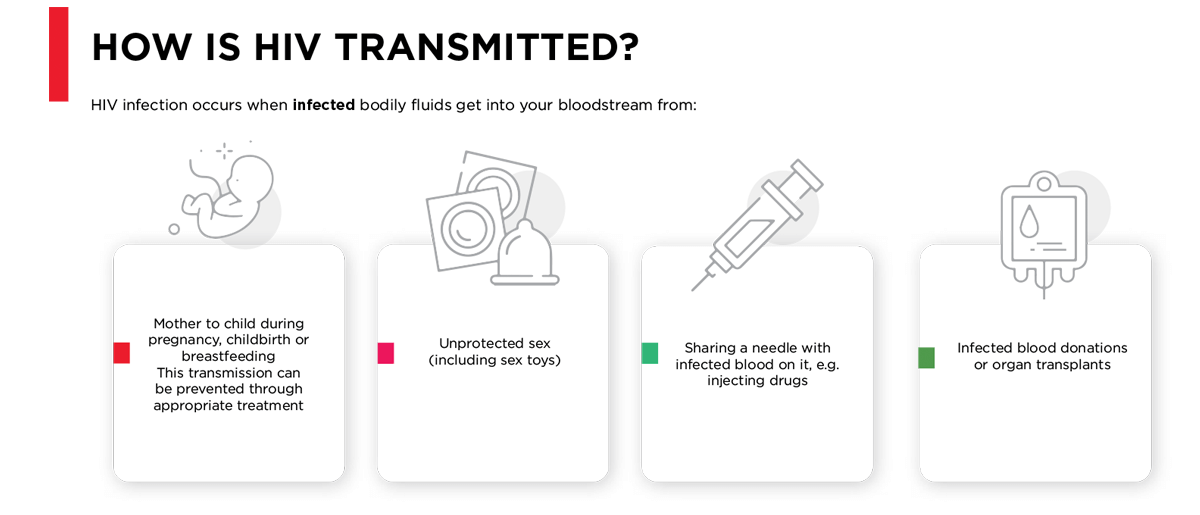
Can I safely have a baby if I’m HIV positive?
A pregnant woman living with HIV can pass on the virus to her baby during pregnancy, childbirth and while breastfeeding. But here’s the good news! Taking antiretroviral treatment correctly during pregnancy and breastfeeding can virtually eliminate the risk of passing the virus on to your baby.
By registering with AfA you will get access to the best clinical care available as well as support through counselling and advice from our trained and experienced staff. Find out more about preventing mother-to-child transmission here.
I know someone who is HIV positive and I’m worried about getting it from them.
It’s natural to want to protect your health, and it’s normal to feel anxious if you don’t have all the facts. You might have heard scary stories or myths from friends or social media. But it’s important to know the truth about HIV transmission so that you can take the right steps to protect yourself without having anxiety about things that aren’t even a risk.
KNOW YOUR HIV FACTS
HIV prevention
There are many ways to prevent the spread of HIV such as:
- Regular HIV testing to ensure you know your status
- Post-exposure prophylaxis (PEP)
- Pre-exposure prophylaxis (PrEP)
- Prevention of mother-to-child transmission (PMTCT)
- Using condoms
- Medical male circumcision (MMC)
Regular HIV testing
HIV testing is voluntary and completely confidential.
A large percentage of new HIV infections are transmitted by people who don’t know they have the virus. For people with undiagnosed HIV, testing is the first step in maintaining a healthy life and preventing HIV transmission.
The South African National Department of Health offers HIV testing at its facilities. And medical schemes as well as many companies in South Africa offer access and funding for HIV testing.
If you get tested and find out that you have HIV, the best thing you can do for your health is to register on AfA as soon as you are diagnosed.
Registration is easy and confidential.
Call us on 0860 100 646.
Send a ‘Please call me’ to 083 410 9078.
Post-exposure prophylaxis (PEP)
PEP must be started as soon as possible after the exposure and within 72 hours. There is no benefit after 72 hours.
PEP is a short-term antiretroviral treatment that reduces the likelihood of HIV infection after exposure to HIV-infected blood or sexual contact with an HIV-positive person.
The aim of PEP is to allow a person’s immune system a chance to provide protection against the virus and to prevent HIV from becoming established in their body. It usually consists of a four-week course of three antiretroviral drugs that are also prescribed as treatment for people living with HIV.
If you have had unprotected sex, been raped or accidentally exposed to blood, you must see your doctor immediately.
Your doctor and the counsellors at AfA will guide you through the process but you should note the following:
- An HIV test should be done as soon as possible after the incident and then repeated at six weeks and three months.
- Until the three-month test is negative, it is important to practise safe sex (including the use of condoms).
- The duration of PEP should be four weeks.
- If you are worried that you’ve been exposed to HIV, please contact AfA immediately for assistance on 0860 100 646 or send a ‘Please call me’ to 083 410 9078.
Pre-exposure prophylaxis (PrEP)
PrEP is a way for people who are at very high risk of getting HIV to prevent infection by taking a pill every day. For example, an HIV-negative person who is in a relationship with an HIV-positive person. If you are exposed to HIV through sex or an injection needle, this medicine can work to keep the virus from becoming permanently established in your body.
When taken daily, PrEP is very effective for preventing HIV but its effectiveness is significantly reduced if not taken consistently. Because PrEP only protects against HIV, condoms are still important for protection against other sexually transmitted infections.
If you want to know more about PrEP, contact AfA on 0860 100 646 or send a ‘Please call me’ to 083 410 9078.
Prevention of mother-to-child transmission (PMTCT)
A pregnant woman living with HIV can pass on the virus to her baby during pregnancy, childbirth and while breastfeeding. But many women only find out they have HIV when they fall pregnant. By this time the unborn child is at risk of getting HIV.
But here’s the good news!
Taking antiretroviral treatment correctly during pregnancy and breastfeeding can virtually eliminate the risk of passing the virus on to your baby. Without appropriate antiretroviral treatment, the chances of HIV passing from you to your baby are between 20-40% during pregnancy and at the time of delivery. The risk of infection increases if you breastfeed. This is one of the reasons why regular HIV testing is so important.
It’s also important to attend appointments with your doctor or healthcare professional regularly during pregnancy so you can receive treatment and medical advice to keep yourself and your baby healthy. Usually, you will be given medicines for the last few months of your pregnancy while your baby will be given medicines for the first few weeks of life.
Babies who are infected with HIV may get sick very often. Even if you’re HIV positive, you can get infected with
HIV again. Protect yourself from getting infected again – always use a condom when you have sex. Getting infected again increases the chance of your baby becoming infected.
If you are HIV negative and have had sex without a condom recently, you need to wait for three months and test again. This is because signs of HIV might not show up in the first test.
If you want to know more about PMTCT, please contact AfA on 0860 100 646 or send a ‘Please call me’ to 083 410 9078.
Using condoms
There are many ways to prevent the spread of HIV such as:
When used correctly every time you have sex, condoms are the best way to prevent HIV and other sexually transmitted infections. They have a very low failure rate and are effective for all forms of sex, including oral and anal sex.
Here are some basic things you can do to make sure you’re using a condom properly:
- Use a new condom every time you have sex.
- Put the condom on as soon as an erection occurs and before any sexual contact, whether vaginal, anal or oral.
- Oil-based lubricants such as Vaseline or baby oil can weaken the condom and increase the chances of it breaking. Water-based lubricants are best.
- A man should withdraw from his partner immediately after ejaculating, holding the condom firmly to keep it from slipping off.
Even if you are HIV positive, you can get infected with HIV again. Always use a condom when you have sex to protect yourself from getting infected again.
The South African government distributes a billion free condoms every year. Free condoms can often be found in workplaces and in public facilities. Condoms can also be bought in pharmacies around the country.
Medical male circumcision (MMC)
MMC has been shown to reduce HIV transmission from women to men by 60%. It is the surgical removal of the foreskin of the penis by a trained healthcare professional or doctor.
Why MMC? The foreskin is more susceptible to HIV compared to other tissue. It has a greater susceptibility to tears and abrasions during sex which makes it easier for infections like HIV, to enter the body. The inner surface of the foreskin is also moist, soft and has a high concentration of target cells for HIV infection.
The moisture also helps HIV to survive. Removing the foreskin through MMC reduces the likelihood of HIV infection.
The South African National Department of Health (NDoH) has endorsed MMC as an HIV prevention strategy for men. It is a voluntary process and the procedure is available free of charge by certain doctors and nurses in the NDoH programme.
If you would like to find out more about MMC or discuss how to access the service, here is a list of links to organisations involved in the national MMC programme:
Aurum
CHAPS
Right to Care
Brothers for Life
National Department of Health
UNAIDS
Centres for Disease Control and Prevention (CDC)
PEPFAR